Cervical Cancer Prevention Week 2022
This year's week of events of highlighting the need for prevention and treatment of Cervical Cancer, takes place from 17th to 23rd January 2022.
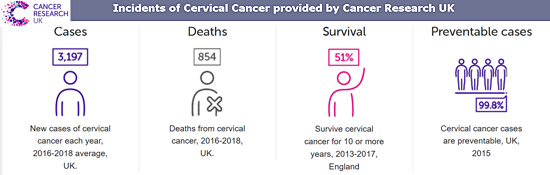
Cervical Cancer can kill if not treated or prevented, and sadly, based on figures for period 2016 to 2018, there are around 850 cervical cancer deaths in the UK every year, that's more than 2 every day.
Yet Cervical Cancer treatment can and does save many lives, as these statistics from Cancer Research UK show:
- Around 8 in 10 (81.1%) of women diagnosed with cervical cancer in England survive their disease for one year or more (2013-2017).
- Around 6 in 10 (61.4%) of women diagnosed with cervical cancer in England survive their disease for five years or more (2013-2017).
 It is predicted that around 1 in 2 (51.2%) of women diagnosed with cervical cancer in England survive their disease for ten years or more (2013-2017).
It is predicted that around 1 in 2 (51.2%) of women diagnosed with cervical cancer in England survive their disease for ten years or more (2013-2017).
- Cervical cancer survival in England is highest for women diagnosed aged under 40 years old (2009-2013).
- Around 9 in 10 women in England diagnosed with cervical cancer aged 15-39 survive their disease for five years or more, compared with around a quarter of women diagnosed aged 80 and over (2009-2013).
- Cervical cancer survival is improving and has increased in the last 40 years in the UK.
- In the 1970s, almost half of women diagnosed with cervical cancer survived their disease beyond ten years, now it's almost two-thirds.
- When diagnosed at its earliest stage, more than 9 in 10 (96%) people with cervical cancer will survive their disease for one year or more, compared with 1 in 2 (50%) people when the disease is diagnosed at the latest stage.
- Five-year relative survival for cervical cancer in women is below the European average in England, Wales and Scotland but similar to the European average in Northern Ireland.
However, awareness of the risk to every female in the country of the causes of Cervical Cancer, has not always been very good at all, with majority of women not having regular cervical smear tests which determine the presence of abnormal cells in the vagina and cervix.
The biggest change to public awareness of the problem and risks of cervical cancer came with the tragic death of reality TV star Jade Goody on 22 Mar 2009 which led to a seismic change in people's awareness of cervical cancer.
 Through her candid interviews she gave about her illness and prognosis, a whole generation of women and girls were suddenly aware of this form of cancer and that it was a major risk to all women and girls, but could be preempted and treated successfully if caught early. Through Jade's campaigning up to her death, the public were made aware and encouraged to get their smear tests regularly.
Through her candid interviews she gave about her illness and prognosis, a whole generation of women and girls were suddenly aware of this form of cancer and that it was a major risk to all women and girls, but could be preempted and treated successfully if caught early. Through Jade's campaigning up to her death, the public were made aware and encouraged to get their smear tests regularly.
After her death in 2009 the number of women having smear tests was 70 per cent higher than expected - saving tens of thousands of lives and changing attitudes towards the disease forever.
Whilst this was for many a sudden awareness of cervical cancer and the need for regular cervical smear tests, sadly as is often the case, once the publicity around Jade's death began to wane, so too did the figures of the number of people taking such tests started to slowly reduce.
Hence why next week's events of public awareness campaigns about cervical cancer are still urgently needed.
Key Facts About Cervical Cancer
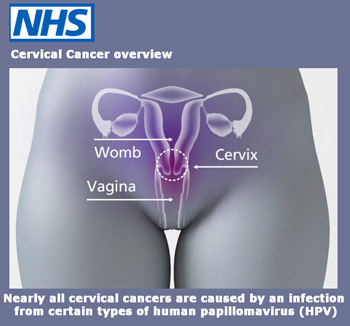
The World Health Organisation provides these key facts about Cervical Cancer and the Human papillomavirus (HPV):
- Human papillomavirus (HPV) is a group of viruses that are extremely common worldwide.
- There are more than 100 types of HPV, of which at least 14 are cancer-causing (also known as high risk type).
- HPV is mainly transmitted through sexual contact and most people are infected with HPV shortly after the onset of sexual activity.
- Cervical cancer is caused by sexually acquired infection with certain types of HPV.
- Two HPV types (16 and 18) cause 70% of cervical cancers and pre-cancerous cervical lesions.
 There is also evidence linking HPV with cancers of the anus, vulva, vagina, penis and oropharynx.
There is also evidence linking HPV with cancers of the anus, vulva, vagina, penis and oropharynx.
- Cervical cancer is the fourth most common cancer among women globally, with an estimated 570,000 new cases in 2018. Nearly 90% of the 311,000 deaths worldwide in 2018 occurred in LMICs (1).
- Comprehensive cervical cancer control includes primary prevention (vaccination against HPV), secondary prevention (screening and treatment of pre-cancerous lesions), tertiary prevention (diagnosis and treatment of invasive cervical cancer) and palliative care.
- Vaccines that protect against HPV 16 and 18 are recommended by WHO and have been approved for use in many countries.
- Clinical trials and post-marketing surveillance have shown that HPV vaccines are safe and effective in preventing infections with HPV infections.
- Screening and treatment of pre-cancer lesions in women is a cost-effective way to prevent cervical cancer.
- Cervical cancer can be cured if diagnosed at an early stage and treated promptly.
However, we now have even better preventative treatment against cervical cancer in the form of a vaccination against the main cause of Cervical Cancer - the Human papillomavirus (HPV) - of which there are over 100 variants.
In the UK, there has been a programme of vaccinations against HPV. Again the World Health Organisation website explains:
Vaccination Against HPV
There are currently 3 vaccines that have been prequalified, all protecting against both HPV 16 and 18, which are known to cause at least 70% of cervical cancers. The third vaccine protects against five additional oncogenic HPV types, which cause a further 20% of cervical cancers.
Given that the vaccines which are only protecting against HPV 16 and 18 also have some cross-protection against these other less common HPV types which cause cervical cancer, WHO considers the three vaccines equally protective against cervical cancer. Two of the vaccines also protect against HPV types 6 and 11, which cause anogenital warts.
Clinical trials and post-marketing surveillance have shown that HPV vaccines are very safe and very effective in preventing infections with HPV infections, high grade precancerous lesions and invasive cancer.*
HPV vaccines work best if administered prior to exposure to HPV. Therefore, WHO recommends to vaccinate girls, aged between 9 and 14 years, when most have not started sexual activity. The vaccines cannot treat HPV infection or HPV-associated disease, such as cancer.
Some countries have started to vaccinate boys as the vaccination prevents genital cancers in males as well as females, and two available vaccines also prevent genital warts in males and females.
WHO recommends vaccination for girls aged between 9 and 14 years, as this is the most cost- effective public health measure against cervical cancer
HPV vaccination does not replace cervical cancer screening. In countries where HPV vaccine is introduced, screening programmes may still need to be developed or strengthened.
Ignorance Is Bliss
 Amazingly, ignorance of both female anatomy and of cervical cancer, still remains highly prevalent amongst the UK population; with many myths circulating. Amazingly, when the HPV vaccination programme first started, there was no major backlash against it from anti-vax groups. Unlike what we see today about Coronavirus.
Amazingly, ignorance of both female anatomy and of cervical cancer, still remains highly prevalent amongst the UK population; with many myths circulating. Amazingly, when the HPV vaccination programme first started, there was no major backlash against it from anti-vax groups. Unlike what we see today about Coronavirus.
However, that does not mean that public health education around cervical cancer prevention and treatment is no longer necessary. As can be seen above with regard to the death of a celebrity, often the shock factor does not last very long.
That being said, the aim of the annually held Cervical Cancer Awareness week is to provide a fact based campaign of education amongst the general public in an attempt to ensure maximum public knowledge of the cause of cervical cancer and of the preventative treatment via the vaccine and the screening programme which is still required in order to cut the number of deaths from the disease.
There are numerous organisations from the NHS to charity organisations such as Jo's Cervical Cancer Trust, and Cancer Research UK which provide detailed information via their websites.
In addition there is a YouTube video available from Cancer Research UK which gives a clear ad simple graphic of the the female reproductive system which is where HPV occurs and leads to cancer of the cervix. Available to view here
This website's E-Library Database has a wealth of information in the form of downloadable documentation which can be accessed by using search words 'cervical cancer' or by using search category 'cancer'.
* Lei et al. (2020) HPV Vaccination and the Risk of Invasive Cervical Cancer. N Engl J Med 2020;383:1340-8. DOI: 10.1056/NEJMoa1917338.
Source: World Health Organisation / BBC / Jo's Cervical Cancer Trust / NHS / Cancer Research UK

